
What is Severe Congenital Protein C Deficiency
WHAT IS PROTEIN C DEFICIENCY?
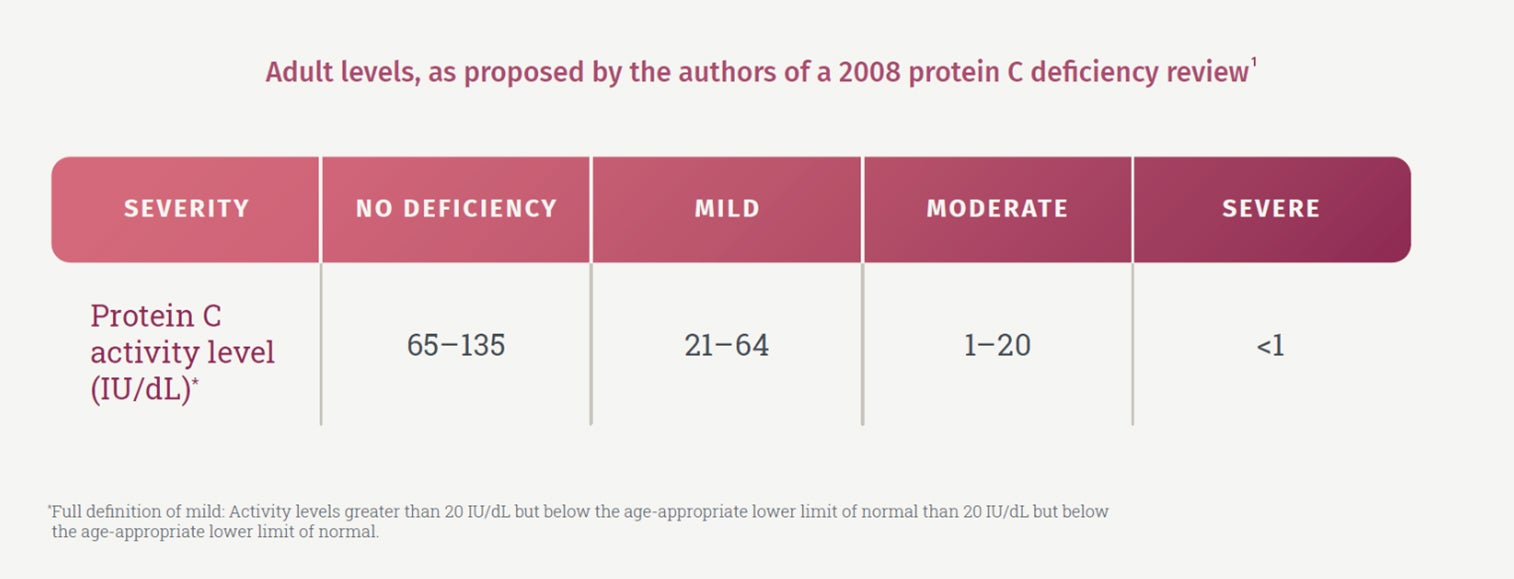
Protein C deficiency can be caused by mutation of the protein C gene (congenital protein C deficiency) or as a result of other conditions (acquired protein C deficiency).1,2 The severity of the deficiency is determined by the remaining plasma activity of protein C.1
Severe Congenital Protein C Deficiency (SCPCD) is an autosomal recessive, rare disorder that leads to high initial mortality and long-term morbidity in survivors.1 In neonates, SCPCD can manifest, within hours after birth, as purpura fulminans with necrosis of the skin and venous thrombosis.1-3
Testing for SCPCD
Several laboratory tests can be conducted upon signs of purpura fulminans to confirm protein C deficiency:
Given possible confounding factors, severe congenital protein C deficiency is confirmed using multiple methods 3
- PROTEIN C (PC) ACTIVITY ASSAY 2,1
- Protein S assay 1 (low PC levels but normal Protein S levels are suggestive of SCPCD)
- Protein C antigen5
- Platelets 5,6
- Fibrinogen 3,5
- D-dimer5
- Prothrombin time (PT) 3,5
- Activated partial prothrombin time 3
- Genetic analysis 3
- Protein C level testing in parents 2 (Protein C activity assay and Protein C antigen)
- PC testing in family members is recommended to determine if the deficiency is genetic and whether it is a homozygous or heterozygous mutation 3
The severity of protein C deficiency is based on protein C activity1
The mean plasma concentration of protein C in a healthy term infant is 40/IU dL, with a lower limit of normal of 25 IU/dL.1
Protein C concentration increases from birth until 6 months of age. Protein C concentration remains slightly low through childhood and achieves the adult range after puberty.1
EARLY DIAGNOSIS OF SEVERE CONGENITAL PROTEIN C DEFICIENCY (SCPCD)
Identification
Clinical diagnosis of purpura fulminans skin lesions is critical3
- Visually identifying skin lesions:
- Infants with SCPCD usually present within hours after birth with rapidly progressive purpura fulminans 3,1
- Because purpura fulminans is a haematological emergency due to the rapidly progressive nature of the multi-organ thrombotic injury, consultation with a haematologist is recommended 2

SCPCD and its potential complications2
- Purpura fulminans can lead to life-threatening complications:
- Purpura fulminans can rapidly progress to organ failure as a result of necrosis and disseminated intravascular coagulation2
- Rates of amputation in infants and children with purpura fulminans may be as high as 62%7

CEPROTIN® is indicated for prophylaxis and treatment of purpura fulminans coumarin-induced skin necrosis and venous thrombotic events in patients with severe congenital protein C deficiency.4
-
Goldenberg N, Manco-Johnson M. Protein C deficiency. Haemophilia. 2008;14(6):1214–21.
-
Chalmers E, et al. Purpura fulminans: recognition, diagnosis and management. Archives of Disease in Childhood. 2011;96(11):1066–71.
-
Price VE, et al. Diagnosis and management of neonatal purpura fulminans. Semin Fetal Neonatal Med. 2011;16(6):318–22.
-
CEPROTIN® 500 IU Summary of Product Characteristics.
-
Khor B, et al. Laboratory tests for protein C deficiency. Am J Hematol. 2010;85:440–2.
-
Tairaku S, et al. Prenatal genetic testing for familial severe congenital protein C deficiency. Hum Genome Var. 2015;2:15017
-
Gürgey A, et al. Outcome in Children With Purpura With Fulminans: Report on 16 Patients. Am J Hematol. 2005;80(1):20–5


